The Science Behind CTE: How Brain Injuries Lead to Long-Term Damage
In recent years, the topic of brain health has vaulted to the forefront of public consciousness, with CTE becoming a particular focal point. CTE, a once obscure medical term, has now become part of our common lexicon, especially within communities connected to contact sports and military service.
But what really lies behind the term CTE? At its core, CTE reveals the fragility of our brain and the profound implications of repetitive trauma to it.
As we explore the intricate mechanisms of this condition, we will gain a clearer understanding of the importance of early detection, the challenges in diagnosis, and the potential avenues for prevention. With the stakes as high as the very essence of our cognition and personality, understanding the intricacies of CTE is not just a scientific endeavor, but a societal imperative.
Understanding CTE
Chronic Traumatic Encephalopathy, or CTE, is a degenerative brain condition believed to result from repetitive brain trauma. Initially, its recognition was primarily among boxers, labeled as “punch-drunk syndrome.”
However, its scope has since broadened, encompassing athletes from various contact sports and even military veterans subjected to blasts. At the crux of CTE is the continuous injury to the brain, even from seemingly mild impacts, which over time can culminate in serious neurological impairments.
Symptoms can vary from memory lapses and mood swings in the early stages to debilitating cognitive and motor deficits as the condition progresses. The insidious nature of CTE makes it both a medical and societal concern, necessitating a deeper dive into its underlying mechanisms.
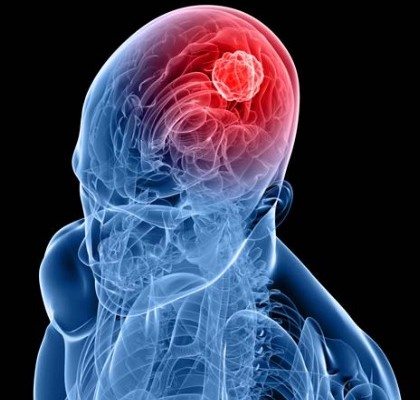
The Anatomy of the Brain and Its Vulnerability
The human brain, an intricate web of nearly 86 billion neurons, is the epicenter of cognition, emotion, and function. Protected by the skull, it appears shielded from external forces, yet its soft, gelatinous nature makes it highly susceptible to injury.
Within this complex structure, neurons communicate through axons, slender thread-like extensions that transmit electrical and chemical signals. When the brain experiences trauma, these axons can stretch, twist, or even break, disrupting normal communication.
Surrounding the neurons are glial cells, the brain’s support system, they provide nourishment, repair damage, and maintain equilibrium. However, repetitive trauma can overwhelm these cells, leading to prolonged inflammation and an inability to repair effectively.
The brain’s delicate composition is further underscored by its intricate vasculature. The blood-brain barrier, a specialized network of blood vessels, serves as a gatekeeper, regulating what enters and exits the brain.
But traumatic forces can compromise this barrier, leading to a flood of potentially harmful substances into the brain tissue.
Mechanics of Traumatic Brain Injury (TBI)
- Types of Head Injuries:
- Concussion: The most common form of TBI, often caused by a direct blow or jolt to the head. It temporarily disrupts brain function, although most concussions do not cause loss of consciousness.
- Contusion: A bruise on the brain caused by an impact, leading to localized bleeding and swelling.
- Penetrating Injury: Caused by an object piercing the skull and entering the brain tissue. These injuries are severe and often life-threatening.
- Diffuse Axonal Injury: Results from violent rotation or shaking of the head, leading to tearing of the brain’s long connecting fibers (axons).
- Immediate Physical Impact:
- Axonal Shearing: Rapid acceleration or deceleration can cause axons to stretch and tear, disrupting neural communication.
- Inflammation: After an injury, the body’s immune response leads to swelling in the brain, which can cause additional damage.
- Cell Death: Traumatic forces can lead to the death of neurons and other brain cells, further compromising brain function.
- Differences Between Single-Incident TBIs and Repetitive TBIs:
- Single-Incident TBI: Often results in immediate and localized damage, with potential for recovery if managed properly.
- Repetitive TBIs: Cumulative damage over time. Even if individual injuries might seem mild, the repeated trauma can lead to lasting and severe damage, increasing the risk of conditions like CTE.
Biochemical Cascade Following TBI
When the brain endures trauma, a series of complex biochemical events ensues. Key among them is the role of tau protein, typically responsible for stabilizing neural structures.
Post-injury, tau can become abnormally phosphorylated, causing it to clump together and form neurofibrillary tangles, a hallmark of CTE and other neurodegenerative diseases. This altered tau can propagate, impacting neighboring neurons and exacerbating neural dysfunction.
After injury, cells release inflammatory mediators, leading to swelling and increased intracranial pressure, which can further harm vulnerable brain tissues. This inflammation, if chronic, can hinder recovery and promote degeneration.
A surge of calcium ions following trauma can damage cells, while oxidative stress can degrade cellular structures and DNA. These biochemical cascades collectively reveal how a singular traumatic event can initiate a sequence of changes, which, when repeated, can culminate in long-term brain damage.
The Evolution of CTE Symptoms
CTE is a covert enemy, often revealing itself slowly over the years or even decades after the inciting traumas. Early manifestations can be subtle, with individuals exhibiting mood disturbances such as irritability or depression, alongside memory challenges or issues with concentration.
As CTE progresses, these symptoms intensify, giving way to severe bouts of aggression, impulse control problems, and profound mood disorders.
In advanced stages, the damage becomes even more palpable. Cognitive deficits mirror those seen in diseases like Alzheimer’s, with pronounced memory loss, confusion, and impaired judgment.
Motor symptoms can also emerge, with some individuals experiencing tremors, gait disturbances, and speech difficulties. Sadly, as CTE advances, it not only robs individuals of their cognitive abilities but also their personalities, relationships, and quality of life, underscoring the imperative need for early recognition, intervention, and prevention.
Prevention and Mitigation
In the realm of CTE, prevention holds paramount importance. Recognizing the inherent risks, many contact sports have revamped guidelines to minimize head impacts. Initiatives include improved helmet designs, stricter return-to-play protocols post-concussion, and enhanced athlete education on recognizing symptoms.
Beyond sports, recognizing and managing potential TBIs in everyday life and military contexts is vital. Post-injury, immediate medical attention and adequate rest are crucial to reduce the chances of long-term complications.
Recent research also delves into therapeutic interventions, including drugs to reduce inflammation or combat tau accumulation. As science advances, the hope is to transform our approach from reactive care to proactive prevention.
Final Thoughts
CTE stands as a testament to the intricate balance and vulnerability of the human brain. With its insidious onset and profound implications, understanding CTE isn’t merely academic—it’s a call to action.
Our increased awareness, combined with advancements in research, paves the way for improved prevention and early intervention. As we navigate the challenges of diagnosis and treatment, it’s imperative for society to prioritize brain health, safeguarding future generations from the long shadows cast by repetitive brain injuries.